Racism is real and stress is not just all in your head.
With genetics-based medicine came the compelling desire to boil every health issue down to one’s DNA, with issues such as hypertension and anxiety falling into an ambiguous field straddling the medical-chart columns for “family history” and “lifestyle.”
“I encountered that medical students here at UF were learning about the supposed genetic basis for racial inequalities in disease. Having been trained as an anthropologist as an undergrad, this seemed crazy to me,” says Lance Gravlee, professor of anthropology. “I had sort of taken for granted that those ideas about race and genes were something of the 19th century, that we had dispensed with that.”
“I had sort of taken for granted that those ideas about race and genes were something of the 19th century, that we had dispensed with that.”
People with darker skin tones may indeed be more likely to have issues with anxiety and high blood pressure, but genetic makeup cannot explain all, which is where Gravlee and fellow professor of anthropology Connie Mulligan come in. They study the effects of racial discrimination and genetics on personal health and aim to find a more complete answer, which lies in the complexities of genetics and its health effects in an environment structured by racism.
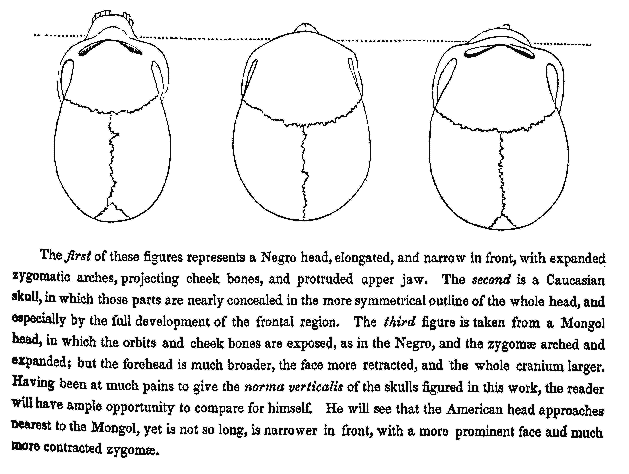
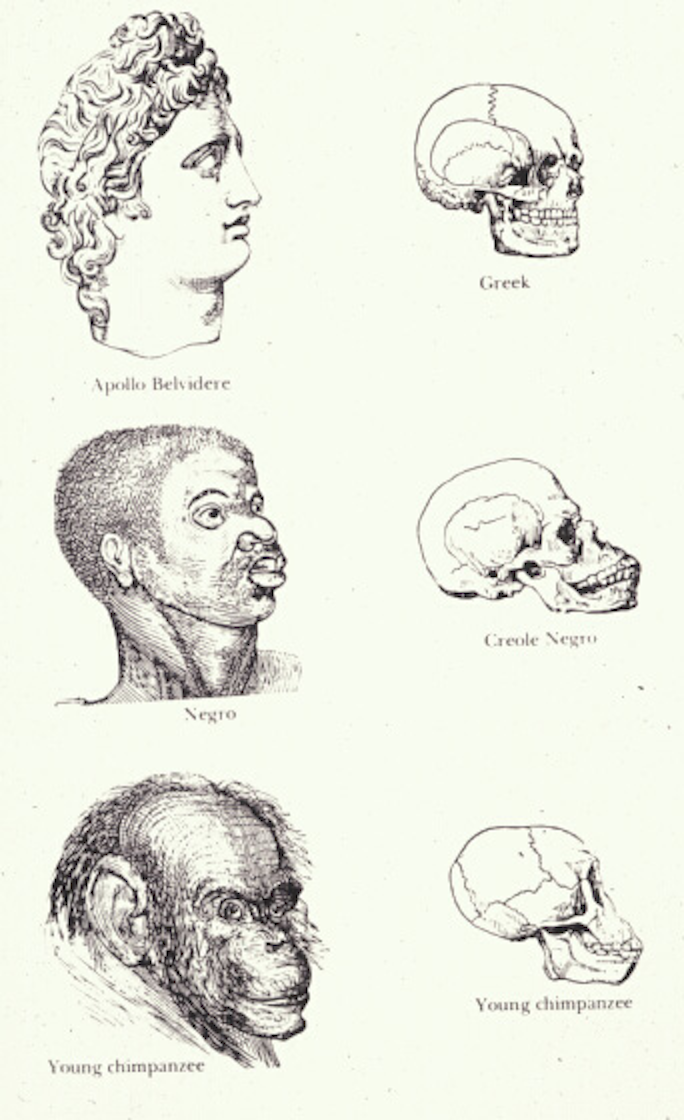
In anthropology’s origins during the 18th century, naturalists developed methods of anthropometry that were designed to classify humans by their race, usually by the size and proportions of their skulls. Modern and ancient skeletons were analyzed through an ever-shifting model of human evolution that meshed with an imperialist spectrum of “primitive” to “civilized” — methods later debunked. However, the notion that one’s skin and blood could fully explain their life and health persisted. After the inception of the Human Genome Project in the mid-1980s, the tendency to conceptualize race and ethnicity — and related health risks — through genetic analysis became popular. These “predictions” seemed to corroborate many health professionals’ observations that certain health conditions were pervasive among people of color. The anthropometric model had been replaced by the ostensibly more scientific, but ultimately restrictive, genome model. Yet the question remained: Was it all in their genes? Of course, it’s more complicated than that.
Meanwhile, anthropologists aimed to “decolonize” their field and shed the racist and imperialist assumptions of their armchair predecessors, which for some meant firmly embracing anthropology’s role as a social science. “In principle, most researchers understand that we need to pay attention to both the genetic and the socio-environmental, but it’s difficult to do that kind of work,” says Gravlee. Possibly exacerbating the difficulty is Western society’s false dichotomy between the mind and the body, as well as the rift between “social studies” and medicine and their respective data sets. “We can sidestep that because we are operating from an anthropological point of view,” says Gravlee. “We understand biology and culture because we have a common language.”
This special perspective allowed Mulligan and Gravlee to complete their groundbreaking project, one that defied that false dichotomy by blending ethnographic and geneticist methodologies. Their paper, published in PLOS ONE (opens in new tab) in 2016, explained that being subjected to racism, even secondhand, was a predictor of hypertension. They identified eight variants in five genes linked to blood pressure regulation, then added sociocultural data to test for associations. When they did, they found a new set of associations with genes known to be linked to depression and anxiety. “Including sociocultural variables opened a new window in biology that we couldn’t see until we took seriously the relevance of those variables,” says Gravlee.
This special perspective allowed Mulligan and Gravlee to complete their groundbreaking project, one that defied that false dichotomy by blending ethnographic and geneticist methodologies.
Their findings show that the overemphasis on genetics excluded a valuable line of inquiry. After the Human Genome Project (opens in new tab)’s completion, genetic determinists expected full answers to all health problems but were left with a concept of “missing heritability,” says Mulligan. If it’s all in the genes, why do some members of a family suffer from heart disease while others don’t? The explanation first requires an understanding of the difference between one’s genes and how those genes are expressed. A genotype is the total set of genes an organism has, while a phenotype is the observed behavior and physical characteristics of that organism. For example, flamingos’ genes do not call for them to be pink; they are pink because they eat mostly carotene-rich shrimp. Gene expression, and therefore phenotype, varies based on several factors, including the environment, which for humans includes the sociocultural realm. “Hypertension is a complex phenotype, like cancer or mental health, yet nobody studies them in that way,” says Mulligan.
Gravlee adds, “Many people who defend race [as a scientific reality] use examples such as a sickle-cell anemia, Tay-Sachs, and cystic fibrosis,” which are associated with people of African, Hebrew, and Northern European descent, respectively, “but those are single-gene disorders.” For complex phenotypes, the answer lies in the field of epigenetics.
Interactions among genetic and environmental factors produce epigenetic effects (opens in new tab) on phenotypes. “Epi-,” a prefix meaning “on top of,” refers to variations in genetic expression that are linked to environmental changes or time. While a person’s “DNA,” as commonly called, or more precisely their genotype, does not change throughout their life, how their cells read those genes does. DNA methylation affects gene expression as a normal epigenetic effect; decreases in DNA methylation have been linked to stress (opens in new tab), by inhibiting expression of genes that code for protein receptors for cortisol. Thus, stress in one’s environment can change their cells’ behavior and have a direct effect on health.
Mulligan’s background in genetics primed her to move into the anthropology of violence and health disparities. “I was tired of looking through the microscope at yeast,” she says. “I love being able to talk to my study organism.” She has progressively immersed herself in the genetics of health since beginning her career in the hard sciences, finally finding intellectual satisfaction at UF.
“Coming into the anthropology department struck me as the biggest sandbox I could play in.” Helping her was Gravlee, who had seen his and others’ colleagues operate under the assumptions that people of color, including those of African or Hebrew descent, were predisposed to certain diseases, and set out to test those assumptions. Gravlee hypothesized that the epidemiology of health disparities had genetic factors; Mulligan hypothesized that the genetics of health included the sociocultural realm. “I like anthropology because I can take the broadest possible perspective on health and what to me is a more accurate — more true — answer in what is driving health and disease,” says Mulligan. Beginning with a meta-analysis of Gravlee’s research in Puerto Rico (opens in new tab) on the relationship between blood pressure variation and perceived skin color, they turned the theoretical into findings. There were indeed interactions between genetic and socio-environmental factors, particularly with regard to racial disparities.
They directed their attention toward Tallahassee (opens in new tab), where Gravlee had been collecting stories of racial discrimination and using social network analysis to study health disparities since 2007. He and Mulligan “envisioned building on those stories to try to develop better measures of the kinds of racism-related stressors that people encountered and see the extent to which we could account for variation in blood pressure,” he says. They chose to continue Gravlee’s study of hypertension because it has long been considered a disease toward which people of African descent are predisposed. Most people understand that stress can cause heart problems, but Mulligan and Gravlee have delved into a type of stress that can be much harder, both socially and politically, to unpack: the stress of racial discrimination. Even asking people to talk about it isn’t cut and dried. “Reports of perceived stress are not good predictors of health outcomes,” says Gravlee.
Gravlee describes his approach as “community-based participatory research.” The project is guided by a steering committee composed of people interested in health equity, the contemporary crux of Tallahassee’s long-running civil rights movement. This situation called for rewriting the Institutional Review Board protocols, which typically require a pre-approved set of questions written by the researcher. However, with their approach, “we were liaisons between community members and the research institution,” says Gravlee. “They are partners, not just participants.” The 100-question survey emerged from conversations with these partners, who guided the researchers in what to ask. This unusual arrangement threw the IRB for a temporary loop, but certainly supports the decolonization of anthropology and demonstrates the potential of oral history and participant-generated research questions to alleviate social inequity.
“Including sociocultural variables opened a new window in biology that we couldn’t see until we took seriously the relevance of those variables.”
Their findings don’t leave much opportunity for researchers in any discipline to hide behind genetic determinism or enforce the divide between biology and culture. “We often equate biology and genes and then regard the environment as something else, something extraneous. People want it to be nature versus nurture,” remarks Gravlee. “Our results suggest that we need a little more nuance.”