
Global Issues — Bug Zappers
Liberal Arts and Sciences investigators at UF’s Emerging Pathogens Institute are here to rid the world of dangerous microbes, wielding state-of-the-art technology with their scientific toolkits of electronic tracking, computer analysis, and petri dishes!
The Geographers:
Professors Gregory Glass and Jason K. Blackburn use telemetry, remote image sensing, and geographic information services data to predict outbreaks of non-viral pathogens.


MALARIA
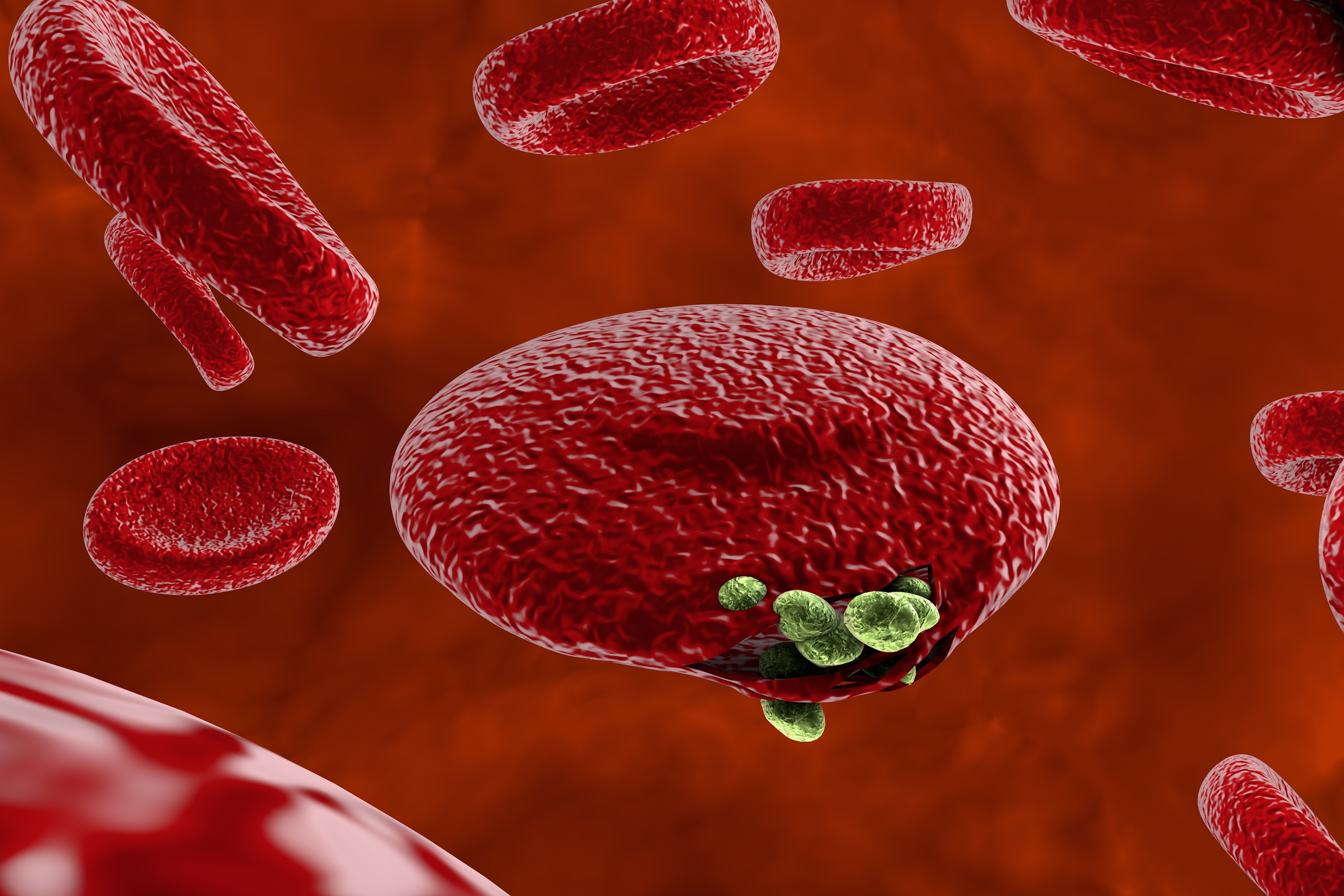 Protozoan. Common throughout tropical and subtropical regions worldwide. Around 200 million cases annually. Mortality rate varies widely depending on location, comorbidity, and demographic.
Protozoan. Common throughout tropical and subtropical regions worldwide. Around 200 million cases annually. Mortality rate varies widely depending on location, comorbidity, and demographic.
Glass uses spatial and climate data to study environmental changes that affect the populations of animals, ticks, and mosquitoes in Florida and around the world. He also collects data on blood testing, insecticides, and other intervention measures to examine their effectiveness.
ANTHRAX
 Bacterium. Common throughout Central and South America and southern Europe. 2,000 cases annually. Threat of weaponization. Mortality rate for intestinal infections is 25 to 75 percent; for respiratory, 50 to 80 percent.
Bacterium. Common throughout Central and South America and southern Europe. 2,000 cases annually. Threat of weaponization. Mortality rate for intestinal infections is 25 to 75 percent; for respiratory, 50 to 80 percent.
Blackburn directs the Spatial Epidemiology & Ecology Research Lab (SEER Lab) and studies how Bacillus anthracis causes anthrax outbreaks among wildlife, livestock, and humans by modeling the pathogen’s ecological niche and transmission mechanisms. To do so, SEER Lab combines GPS technology to track animals, such as elk and bison, and laboratory work to study environmental conditions that promote B. anthracis spore persistence. Blackburn works with UF ecologists Jose Miguel Ponciano and Robert Holt in an NIH-funded project to study environmental reservoirs and anthrax transmission.
The Biologists:
Professor Derek Cummings and research assistant Kyra Grantz use statistical analysis of sociodemographic data to monitor and predict the spread of disease.


DENGUE
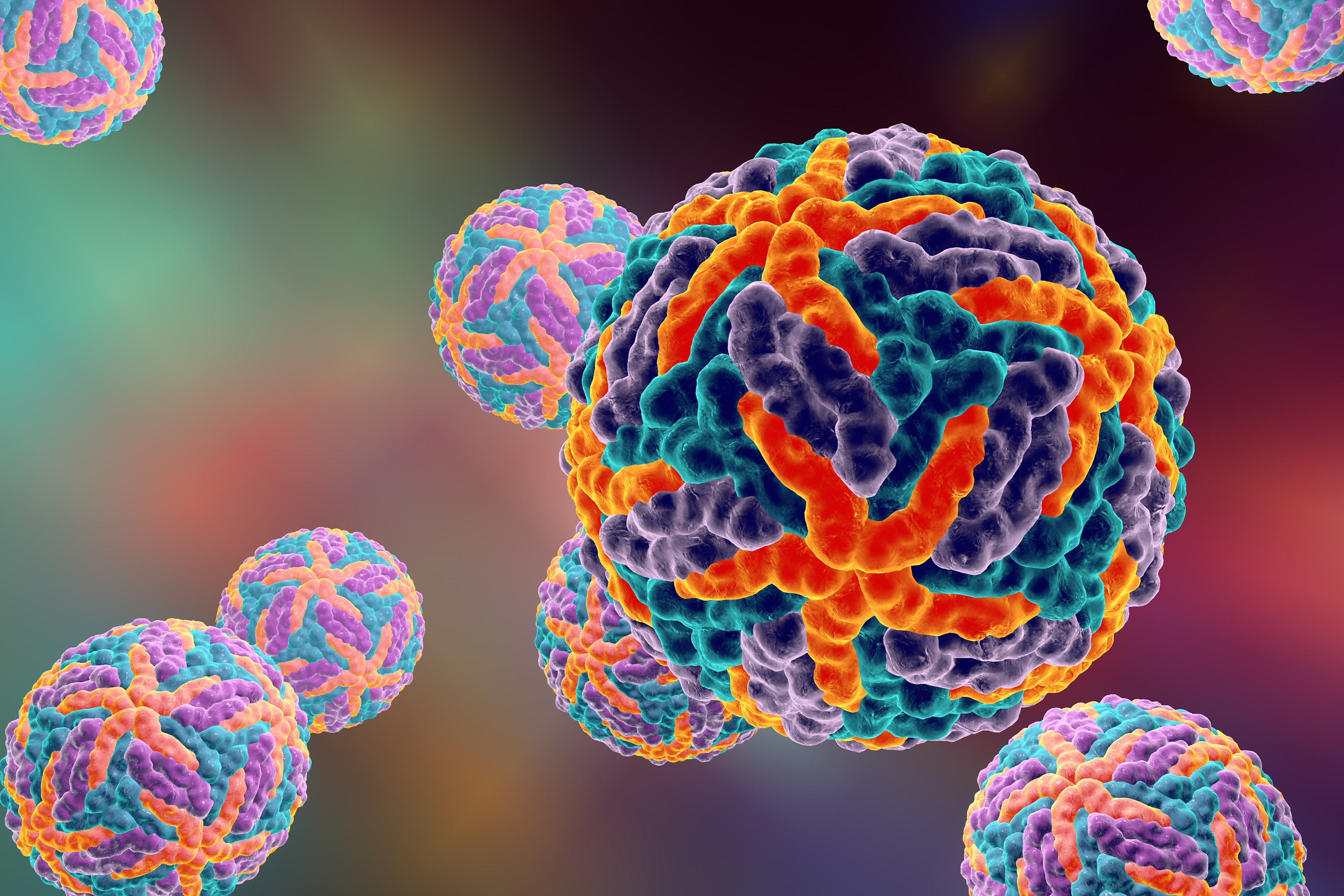 Flavivirus. Endemic to Puerto Rico, common throughout Latin America and Southeast Asia. 50 – 528 million cases annually. Mortality rate is 1 percent.
Flavivirus. Endemic to Puerto Rico, common throughout Latin America and Southeast Asia. 50 – 528 million cases annually. Mortality rate is 1 percent.
Cummings has worked on risk models of the new dengue vaccine, called CYD-TDV and trademarked Dengvaxia. People experiencing their second natural dengue infection have a higher risk of severe symptoms than those with their first infection. After two infections, however, the risk of severity decreases. Because the vaccine imitates a natural infection, it works best in areas where people have already been exposed to the virus. Given the dangers associated with vaccinating someone who has never been exposed to dengue virus, Cummings recommends a point-of-care screening tool that could identify those who have been infected in the past.
INFLUENZA
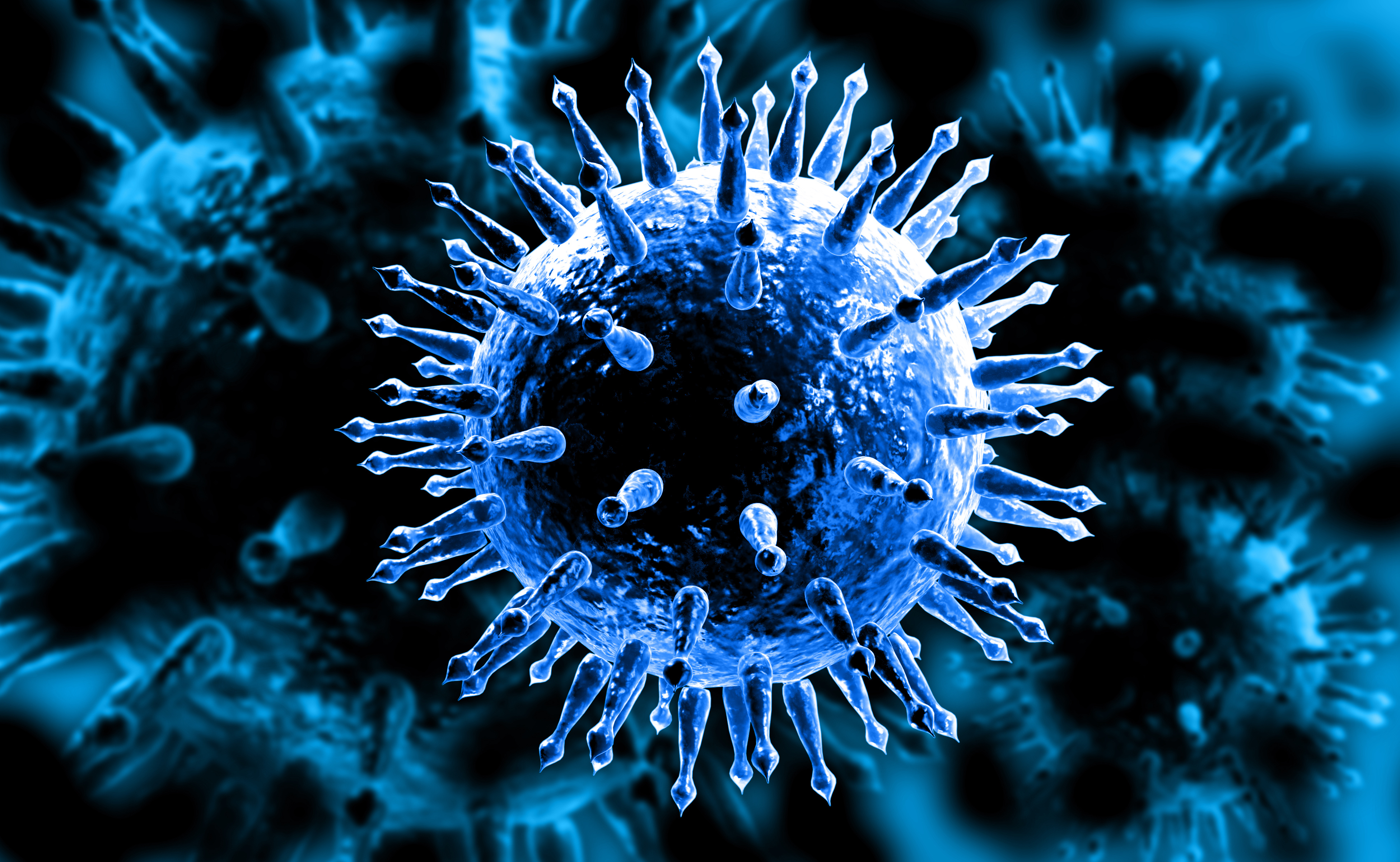 RNA virus. Worldwide, occurs in annual outbreaks, with rare pandemics. 3 to 5 million cases annually. Mortality rate is 1.5 percent.
RNA virus. Worldwide, occurs in annual outbreaks, with rare pandemics. 3 to 5 million cases annually. Mortality rate is 1.5 percent.
In 1918, an unusually deadly flu swept the world, claiming 50 to 100 million lives in a pandemic often called the Spanish flu. Grantz studies how sociodemographic markers and urban infrastructure affected the spread of the flu in Chicago in that terrifying year. Analyzing 100-year-old data collected by the U.S. Census and the Chicago Department of Health, she’s found that mortality rates increased with illiteracy and unemployment and decreased with homeownership. She developed a technique to model the spread of infectious disease and found that increased likelihood of mortality can be determined on a meter-by-meter basis. This finding suggests that neighborhood-level outbreaks are a vulnerable point in epidemic control.


